Reducing Mental Illness in Rural Jails
Introduction
DownloadsPrintable PDF
Letter from the National Association of Rural Mental Health (NARMH)
Letter from the National Sheriff's Association (NSA)
County Case Studies
Jump to SectionCounties Use the Sequential Intercept Model to Identify Potential Changes
What Happens Inside a Jail Can Be Just as Important as Outside
Sharing Resources Helps Neighbor Counties Do More
Counties Seek Quality, Affordable Housing for People with Mental Illnesses
Conclusion
Codington County is "Stepping Up"
U.S. jail admissions reach 11 million annually, and the number of people in county jails is now at four times the size of the 1970 jail population. Much of this growth has been driven by small and mid-sized counties, which now make up more than 75 percent of the U.S. jail population.1 Jails across the nation serve an estimated 2 million people with serious mental illnesses each year2 – almost three-quarters of whom also have substance use disorders.3 The prevalence of people with serious mental illnesses in jails is three to six times higher than for the general population.4 Once incarcerated, these individuals tend to stay longer in jail and upon release are at a higher risk of returning than those without these illnesses.
The human toll – and its cost to taxpayers – is staggering. Jails spend two to three times more on adults with mental illnesses that require intervention than on people without those needs,5 yet often do not see improvements in recidivism or recovery. Despite counties’ tremendous efforts to address this problem, they are often thwarted by significant obstacles, such as coordinating multiple systems and operating with minimal resources. Without change, large numbers of people with mental illnesses will continue to cycle through the criminal justice system, often resulting in missed opportunities to link them to treatment, tragic outcomes, inefficient use of funding and failure to improve public safety.
Despite their small populations, rural counties face some of the same challenges as urban counties. Rural counties have residents with mental illnesses, they lack enough resources to provide quality services and they face the same legal and policy barriers to implementing new programs and practices as their more populous counterparts. But in some ways, rural counties struggle even more:
- Access to Community Services: With so few resources, many rural counties don’t have any mental health treatment providers of their own – or a jail, for that matter – and are forced to partner with nearby counties to share resources. As a result, county residents may have to drive hours to receive services, making the lack of transportation options in these areas even more salient. In some places there may be only one service provider covering six counties. If that provider refuses to work with people who have been or are currently involved in the criminal justice system, there is often no option left but a jail when a person is in crisis.
- Providing Jail Mental Health Services: It is hard enough to provide mental health services inside a large jail in a more urban area where mental health providers are more accessible, but in rural jails – many of which may only have the capacity to hold a few people at a time – the possibility of implementing mental health services behind the walls is unlikely, if not impossible, due to the lack of services generally within the county or region and the small jail staff and facilities.
- Providing Housing for Residents with Mental Illnesses: Most counties struggle with providing adequate, quality and affordable housing for people with mental illnesses. As a result, many individuals with severe and persistent mental illnesses will experience homelessness within their lifetime.6 Rural counties in particular lack diverse and affordable transitional and permanent housing options for people with mental illnesses, especially those with previous criminal justice involvement.
The goal of this publication is to provide rural county leaders with ideas and strategies for addressing these challenges by providing examples of counties that have successfully done so or are making progress. There is no one strategy that will work for all counties, or all rural counties. But county leaders are encouraged to learn from each other’s experiences and adapt their peers’ policies, practices and programs to fit the needs of their county and residents.
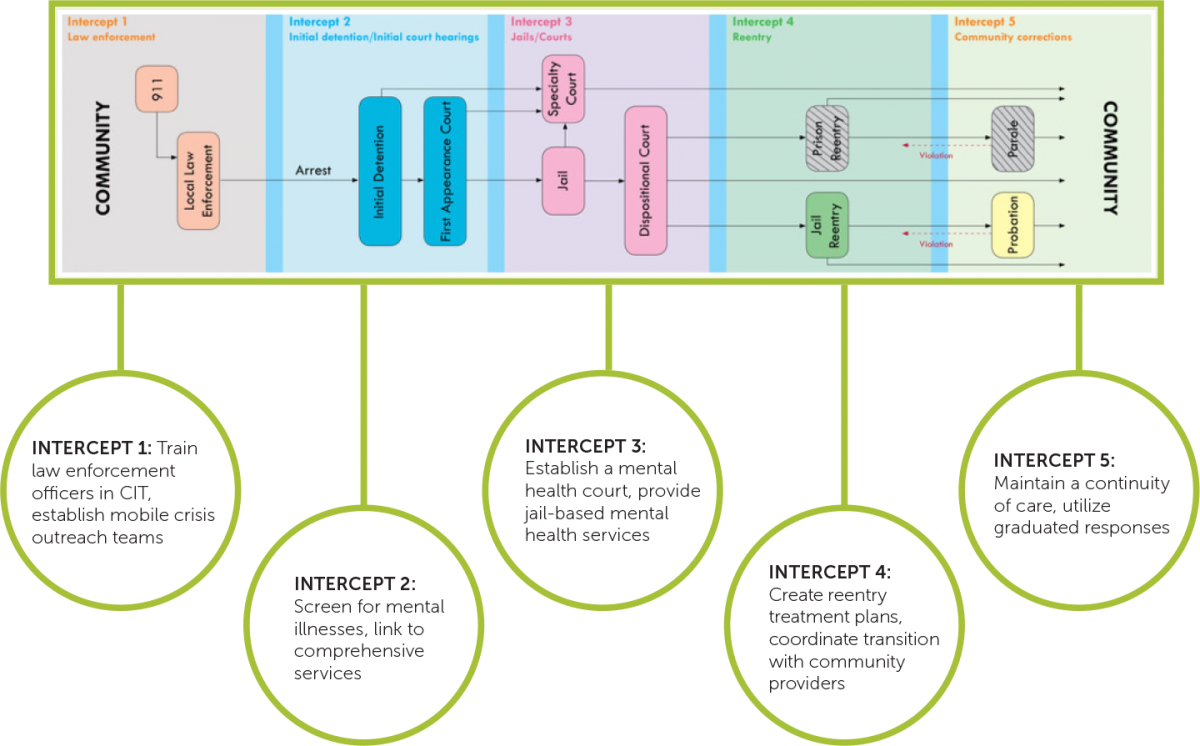
Counties that have implemented individual programs or policies to address the number of people with mental illnesses in their jails often realize that there are multiple points where changes need to happen to have a real impact. The Substance Abuse & Mental Health Services Administration’s (SAMHSA) GAINS Center recognized this and developed a model to help jurisdictions organize the way they approach strategies at these different points. The Sequential Intercept Model provides a basis for thinking about the five intercept points (law enforcement, initial detention/initial court hearings, jail/courts, reentry and community corrections) and how counties can make changes at each to impact the number of people with mental illnesses coming to and staying in their jails.7
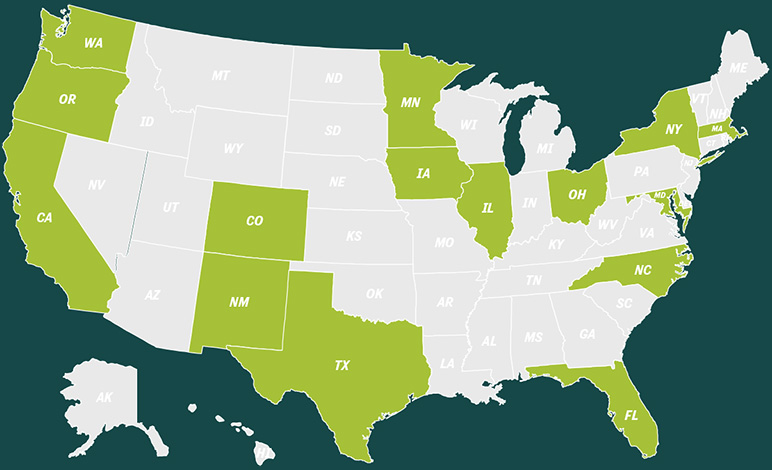
Diverse counties of all sizes from across the country have used the Sequential Intercept Model to identify points in their system where they could implement new policies, practices or programs. Below are examples of each intercept.
I fully support our county’s efforts to reduce the number of people with mental illnesses in our jail,” says Dunn County Chairman Steve Rasmussen. “This is fundamentally a medical issue; we wouldn’t lock up someone who was in a diabetic coma. It’s the right thing to do. It is also the enlightened, wise and compassionate thing to do for our residents. It addresses the reality of the situation we face in our county and also has a side benefit of helping to manage the rising costs of our public safety system.
Dunn County, Wis., used the Sequential Intercept Model to identify several mechanisms to support diversion to community services as a way to address the increasing number of individuals with mental illnesses admitted to hospital emergency departments and jails. These mechanisms included implementation of mobile crisis teams and an integrated treatment court for people with co-occurring mental illnesses and substance use disorders, amongst other services. In addition, the County Board of Supervisors passed a resolution to participate in the Stepping Up initiative in May 2015. Since then, staff has been engaged in Stepping Up technical assistance resources and is developing a process for better calculating mental health prevalence rates and using this information to inform next steps for meeting the needs of this population before they come to the jail.
The Jail Alternatives Program here in Johnson County has not completely alleviated our need for more jail beds, but it has alleviated a lot of the need and more importantly, people are now being served in a much more appropriate way,” notes County Supervisor Rod Sullivan. “We on the County Board are 100 percent bought in to jail alternatives. They work. Not only do they work in terms of keeping people out of the jails, but it’s the way that people should be treated. It’s a total win-win. We fully support our county in doing more to serve this population, because we’ve seen the results here and they are very good.
Johnson County, Iowa, also used the Sequential Intercept Model to develop interventions at key intercept points such as jail screening processes and hiring two jail alternatives coordinators to provide referrals and case management with the ultimate goal of diverting individuals before they become involved in the justice system and identifying and intervening with those who are already involved in the system. The County Board of Supervisors passed a resolution to participate in the Stepping Up initiative in August 2015 and has since been engaged in technical assistance resources and opportunities through the initiative. One of their next steps is to develop a plan for working with residents who are the most frequent users of their services.
Despite counties’ best efforts at keeping people with mental illnesses out of jails, situations arise where these individuals are still detained. Sheriffs across the country struggle with maintaining safe environments for all of their detainees, especially for those with mental illnesses. Jails were never designed as therapeutic environments for individuals, or to house them for long periods of time. However, with jails often being utilized as mental health hospitals – both in rural and urban areas – due to a lack of community resources, sheriffs frequently find themselves in this position. A number of rural counties have implemented effective policies, procedures and programs within their jails to help meet the needs of individuals with mental illnesses while they are detained and to set them up for success when they leave.
We are proud of what we have done here in the Luna County Detention Center,” says Luna County Commission Chair Joe L. “Oleo” Milo, Jr. “Mental health issues in local detention centers are arguably the single largest liability local governments face in today’s world. As a commissioner, it’s not just about the liability. The human component must be paramount in making decisions related to these individuals. This one issue covers the entire spectrum of my job as a commissioner. Being able to solve liability issues through improving the quality of life of these people is a great feeling.
In Luna County, N.M., a geographically large county located in the southwest corner of New Mexico along the Mexico border, the new jail director realized that lack of access to mental health services in the jail was leading to high recidivism rates. He worked with county leadership to hire a full-time licensed mental health therapist to conduct assessments and provide mental health services inside the jail and is currently exploring the opportunity for implementing telepsychiatry in the jail. The jail has also trained staff on Mental Health First Aid and implemented its own jail-based Crisis Intervention Team (CIT). They are currently piloting a reentry planning program to connect people to community-based services upon release.
I couldn’t be more proud of the work the Merrimack County Department of Corrections is doing with its staff and its collaboration with community partners to reduce recidivism and better serve people with mental illnesses who come into contact with our jail,” says Merrimack County Commissioner Bronwyn Asplund-Walsh. “My hope is that ours will become a model for the rest of New Hampshire and the nation on how to treat people with mental illnesses.
In 2011, the Merrimack County, N.H., Department of Corrections partnered with the courts, law enforcement and mental health providers to develop a series of programs to help reduce the number of people with mental illnesses in their jail and provide better services for these individuals while detained and when leaving the jail. They developed the only jail-based Crisis Intervention Team (CIT) in the state and provide case management and psychiatric services in the jail. They are also currently in the process of re-purposing the old jail facility into a community corrections reentry center for men and women that will offer work release programming, gender-specific treatment and services and SOAR (SSI/SSDI Outreach, Access and Recovery), a benefits enrollment program, to better connect people to community-based services for their behavioral health needs.9 Merrimack County also recently passed a resolution to participate in the national Stepping Up initiative.
State Innovations in Health Care for People with Mental Illnesses
At least 15 states have passed laws allowing for suspension rather than termination of Medicaid benefits for individuals who are detained or incarcerated in correctional facilities.8 As a result, jails across the country can keep individuals enrolled or do presumptive eligibility with individuals to get their Medicaid ID before they are released, making it easier to set up appointments and call in prescriptions to be ready once they return home. Even when an individual is only detained for a short period of time staff is able to get the process started for enrollment.
Frequently, smaller or more rural counties do not have the resources to appropriately and effectively serve individuals with mental illnesses. Regional behavioral health authorities and providers and regional jails are common occurrences in these areas. These regional partnerships and resources provide opportunities for counties to share services to reduce individual costs and make the most of what is available. Not every county needs or can afford its own hospital or treatment program. Regional partnerships provide opportunities to share funding and resources to have the largest impact on county residents.
The scope of challenges that need to be addressed regarding persons with mental illness and chemical dependency diagnoses in jails and rural settings are significant,” says Aitkin County Commissioner Anne Marcotte. “Aitkin County has established programing wherein Aitkin County Health and Human Services and the county jail work together to bridge the gaps between release and provider services which has made, and will continue to make, a remarkable difference to the client and the community as a whole. With such innovative ideas being implemented, the crisis of meeting the needs of those with mental illness should continue to be lessened.
The New River Valley in rural southwest Virginia implemented the first regional Crisis Intervention Team (CIT) program in the country,10 representing four counties (Floyd, Giles, Montgomery and Pulaski), one small city (Radford) and 14 law enforcement agencies ranging in size from two officers to more than 100. In addition to training law enforcement officers how to effectively respond to individuals experiencing mental health crises, the regional partnership created a therapeutic crisis assessment center. Law enforcement officers can take individuals in crisis to the center and transfer custody to allow for immediate evaluation and triage in a therapeutic, rather than law enforcement, setting.
In 2009, six counties in central Minnesota (Aitkin, Cass, Crow Wing, Morrison, Todd and Wadena) formed a regional partnership to provide mobile behavioral health services in homes throughout the region and train law enforcement officers how and when to access these services when responding to mental health crisis situations.
Finding quality, affordable housing is consistently one of the biggest challenges identified by people with mental illnesses. According to SAMHSA, about 30 percent of people who are chronically homeless have mental health conditions and half of those also have co-occurring substance use disorders.11 In comparison, only 6 percent of Americans have a severe mental illness. Counties struggle with identifying housing for these individuals, especially when they are currently or have been involved in the criminal justice system. This is particularly true for rural counties where options for temporary housing or repurposing of existing housing are rare if not nonexistent.
There is a mental health crisis in todayâs society,â says El Dorado County Supervisor Sue Novasel. âEl Dorado County is working to address the issue by transitioning mental health patients from our jails and into normal living conditions. A critical component for productive treatment is housing, where individuals and groups can feel safe, settled and secure, and where they can maximize their opportunities for success. Transitional housing gives all concerned a chance to turn crisis into care.
In September 2015, El Dorado County, Calif., a geographically large county located along the Sierra Nevada mountains on the Nevada border, opened a transition house specifically for individuals with the most acute mental health needs who are also involved in the criminal justice system – the only house in the county with a specific focus on this population. Once admitted to the house, individuals are assigned an intensive case management team that works with the Behavioral Health Court and probation to develop a treatment plan and provide full services to help people get back on their feet.
Newark, Ohio, just east of Columbus, is home to the Main Place, a 501(c)3 consumer-operated mental health recovery center that provides services to residents of Licking and Knox counties. The center is operated for and by persons experiencing serious and persistent mental illnesses (SPMI), many of whom have previous or current criminal justice involvement. After exploring the local availability of housing resources in the area, the center established a process through which the subsidy that supports that housing can change from emergency housing to transitional housing, to Shelter Plus Care to Section 8. This allows adults with SPMI to obtain a place to live and stay there as long as they wish. The center also established 10 units of permanent supportive housing where residents participate in activities and treatment at the Main Place and with other community-based behavioral health service providers.
Conclusion
Rural counties, like all counties, face significant obstacles when trying to effectively serve residents with mental illnesses. Counties across the country have built collaborative county and regional partnerships to address these obstacles and demonstrated positive results. As rural counties move forward with their initiatives, whether through Stepping Up or on their own, the hope is that they will be able to learn from the experiences of their peers and work together to reduce the criminalization of people with mental illnesses in their communities and nationwide.
Codington County is a geographically large rural county on the east side of South Dakota. The County Board of Commissioners passed a Stepping Up resolution in June 2015. Commissioner D. Lee Gabel from District 1 was interviewed about the countyâs intentions with the initiative.
Why Did Codington County Pass a Resolution?
Codington County has been facing a number of challenges recently with our court caseload and jail population. We have an aging and small jail that is not meeting the needs of our county. The state has really begun to focus on reducing the state penitentiary population, so criminal justice reform is on everyoneâs mind here. So in that context, there was already some political will to do something. When Stepping Up highlighted the issue of mental illness in jail, my fellow commissioners and I were receptive. Our Welfare Director did her homework and suggested the Stepping Up resolution to the Board with support of the Sheriff. The initiative seemed like it would help us address some of our challenges in our jail. After some discussion, we adopted the resolution unanimously.
Was there any disagreement or pushback about joining the initiative?
Because of the problems we are facing with our jail and the population, we didnât face a lot of opposition to getting involved. I was concerned about passing a resolution with only good intentions, but once I understood the resources that were available to us through the initiative â all of the webinars and other tools â I was persuaded. We wanted to make sure that passing this resolution was going to result in real work being done to address this issue, and it has so far.
What has Codington County been doing to address this issue since passing the Stepping Up Resolution?
We are very fortunate to have someone in our county â our Welfare Director â who has been able to really focus on this issue and help move things forward with the initiative. We have developed a small Stepping Up working group consisting of myself, the Welfare Director, the Sheriff, the Chief Corrections Officer, the community mental health center and our new jail mental health professional. As a result of having access to expertise through Stepping Up, we were able to quickly identify an action that we could take immediately to get the initiative moving. We hired a part-time mental health professional to provide services at the jail. He works 20 hours per week and both the staff and the inmates at the jail have already responded well to having him on site. Anecdotally, he sees about eight inmates per day, which also shows us the extent to which this is a problem in our jail.
We are currently in the process of trying to better identify people with mental illnesses who come into the jail by researching screening tools and strategizing ways to best systematize this process. We want to make the process efficient and effective, while collecting data and developing outcome measures to accurately understand our efforts. We have already seen some positive results, but we want the data to show it and to help guide us in our next steps.
What are you hoping to do through Stepping Up
The end goal is really to have a well-operating system that is able to effectively identify people with mental illnesses who come into the jail and have options available to ensure that only the people who need to be in the jail are detained there and those who donât can be connected to services in the community. We are currently working to bring in additional stakeholders to help meet this need. We would also like to minimize the time that individuals spend in our jail pretrial, and provide them with the services they need to ensure that they are better connected to the community once they leave. We want to effectively use our resources for the individuals who need them most. We know that this process is going to take some time, but we are willing to put in the time to do it right.
Getting Started
Counties seeking to start an initiative to reduce the number of people with mental illnesses in their jail may find the task so daunting that they struggle with where to even start. The Stepping Up initiative provides step-by-step guidance and resources for how to get started on a local initiative or how to continue or enhance this process. Counties differ greatly in terms of their structures and leadership, as well as their available resources and opportunities. Stepping Up was designed to meet all counties – big and small – where they are and to help move them to where they want to be.
Through Stepping Up, resources such as webinars and planning exercises are available to help guide counties through this process. All of these resources are available on the Stepping Up website at www.StepUpTogether.org/Toolkit. More resources and learning opportunities are being added regularly to assist counties that want to make a difference for their residents.
To learn more about the Stepping Up initiative or to join the Call to Action by passing a resolution or proclamation, go to www.StepUpTogether.org or contact Nastassia Walsh, Program Manager, County Solutions and Innovation, NACo, with any questions at nwalsh@naco.org or 202.942.4289.