The County Maternal Health Landscape: Inequities, Barriers and Recommendations

Upcoming Events
Related News
Counties play a critical role in improving the health of pregnant and postpartum people. As owners and administrators of the local health and human services social net, county leaders recognize that rising instances of maternal health complications and deaths underscore the necessity for enhanced provision and accessibility of maternal health services. Further, disparities in maternal health experiences pose a serious equity issue that can be addressed through policies and programs that lead to strong birth outcomes.
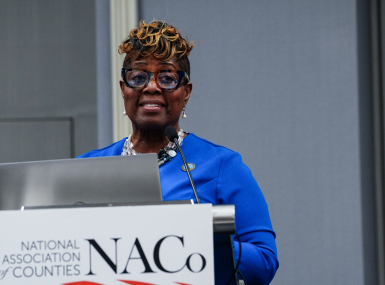
To better understand the challenges and opportunities for county government in supporting pregnant and postpartum people, the National Association of Counties Research Foundation (NACoRF) surveyed county officials on their role and authority in maternal health, gaps and barriers in maternal care systems and county-level solutions and priorities. This report highlights survey findings alongside focus group and interview responses to share the critical role of counties in serving pregnant and birthing residents. County leaders can use this information to guide development of comprehensive, accessible and equitable local maternal health care systems.
Staff Contacts
Advocacy
Federal Actions on Key Maternal Health Policy Priorities: An Overview for Counties
Across the country, counties are facing a critical maternal health crisis. According to March of Dimes, 4.7 million birthing people live in counties with limited maternity care access.

Related News
Prince William County transforms crisis care through "No Wrong Door" approach
Prince William County, Va.’s Crisis Receiving Center is bridging the gap between emergency room care and traditional outpatient care in behavioral crisis response and reducing burden on local law enforcement and hospitals.

Federal-level child welfare priorities center on supporting foster youth, families
Child welfare experts outlined current priorities at the federal level, including better supporting foster care youth who age out of the system and recruiting more foster parents, at NACo’s Human Services and Education Policy Steering Committee meeting.

House Agriculture Committee introduces 2026 Farm Bill
On February 13, House Agriculture Committee Chairman G.T. Thompson (R-Pa.-15) introduced the House version of the 2026 Farm Bill, the Farm, Food, and National Security Act of 2026.

