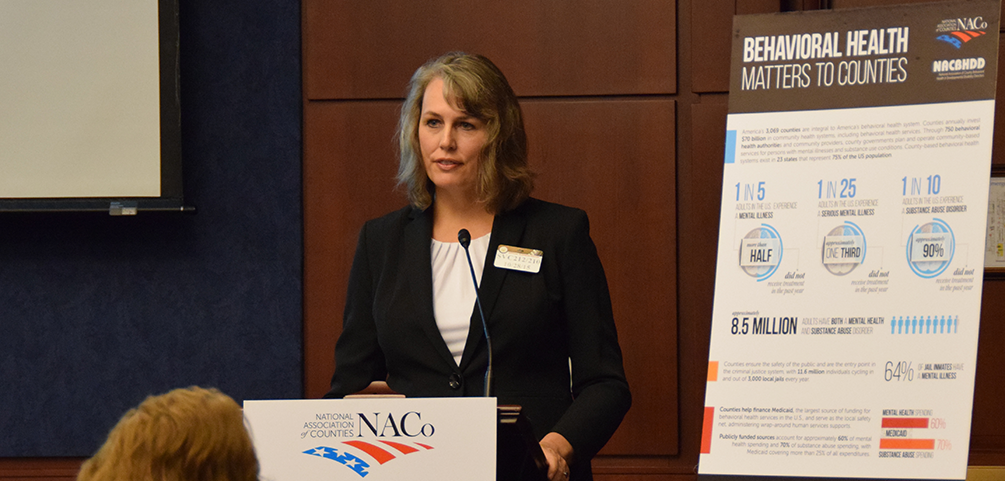
NACo briefs Congress on behavioral health issues
Upcoming Events
Related News
Attachments
Related News

House Agriculture Committee introduces 2026 Farm Bill
On February 13, House Agriculture Committee Chairman G.T. Thompson (R-Pa.-15) introduced the House version of the 2026 Farm Bill, the Farm, Food, and National Security Act of 2026.

Drug tracking software helps counties identify trends, save lives
Florida counties are using an artificial intelligence tool called Drug TRAC to track and report drug trends, with the aim of providing quicker outreach and saving lives.

White House Executive Order establishes national substance use disorder response
On January 29, the White House issued an Executive Order (EO) establishing the Great American Recovery Initiative, a new federal effort aimed at coordinating a national response to substance use disorder (SUD).